
Migraines can disrupt your life, sidelining you with throbbing pain, nausea, and sensitivity to light. At Prestige Health and Wellness, we believe in more than symptom relief—we focus on addressing the root causes of migraines. Treatments like chiropractic adjustments, massage therapy, acupuncture, and physical and occupational therapy can help reduce the frequency and intensity of migraines by relieving tension, improving alignment, and restoring balance to your body. Discover a personalized approach to managing migraines and reclaiming your well-being.
Are You Struggling with Migraines? Find Relief with Chiropractic and Holistic Treatments in NYC
Understanding Migraine Headaches
Migraines are complex neurological events that progress through distinct stages. Symptoms vary from one migraine to another and between individuals.
Prodrome Stage (Pre-migraine):
- Subtle changes signal an impending migraine.
- Food cravings
- Unexplainable changes in mood
- Yawning uncontrollably
- Fluid retention
- Increased urination
Aura Symptoms:
Auras appear from 10 minutes to an hour before the actual headache, lasting for about an hour.
- Visual: Flashing lights, haze, or zig-zag patterns.
- Touch: Tingling or numbness.
- Speech/Language: Difficulty speaking or understanding.
- Motor: Weakness or paralysis on one side of the body or face.
- Brainstem: Coordination issues, balance problems, vertigo, tinnitus, or digestive changes (e.g., diarrhea, constipation).
- Retinal: Partial or total blindness in one eye or shimmering visual effects.
Headache Phase:
- One-sided, pulsing pain.
- Moderate to severe pain that worsens with physical activity.
- Nausea
- Vomiting
- Sensitivity to light (photophobia) and sound (phonophobia).
Postdrome Stage (Aftereffects):
- Difficulty concentrating
- Dizziness
- Exhaustion
- Confusion
- Mood changes
What Causes Migraines and Headache Pain?
Migraine triggers can vary greatly from person to person, but certain factors are commonly known to set off an attack. Understanding and identifying these triggers is key to preventing or reducing the frequency of migraines. While not all triggers will affect everyone, being mindful of these factors can help patients manage their condition more effectively.
Common Migraine Triggers
- Stress: Research shows that 80% of cases are affected by stress. Emotional or physical stress is a frequent cause of migraines, making stress management important.
- Sleep disturbances: Irregular sleep patterns or insufficient sleep can trigger migraines. Establishing a consistent sleep schedule can be helpful.
- Hormonal changes: Hormonal fluctuations, particularly during menstruation or menopause, are linked to increased migraine risk.
- Certain foods: Aged cheeses, processed meats, alcohol, and caffeine are known to trigger migraines in some individuals.
- Weather changes: Shifts in weather, such as temperature or barometric pressure changes, can provoke migraines.
- Strong smells and bright lights: Sensory stimuli like strong perfumes or intense lighting can lead to migraines.
- Skipping meals: Extended periods without eating can lower blood sugar levels, triggering an attack.
- Posture and physical strain: Poor posture or physical strain, such as neck tension, can lead to migraines.
The Cervical Spine, TMD, and Their Role in Headache Pain
Nerve Roots and Meninges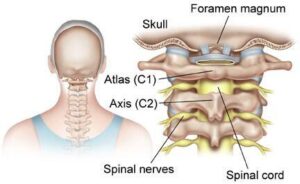
The cervical spine plays a key role in migraine development, particularly the C1, C2, and C3 nerve roots. These nerve roots send pain signals from the head and neck and interact with the meninges, the protective layers around the brain and spinal cord. These layers house blood vessels that can become inflamed during a migraine, contributing to pain.
Nerve Roots and Pain Transmission
The C1-C3 nerve roots transmit pain signals to the trigeminocervical nucleus, which processes pain from the face and the neck. This connection explains why neck problems can lead to headaches or facial pain. For instance, stimulating the C1 nerve root can cause pain behind the eyes, a common migraine symptom.
The Meninges and Migraine Pain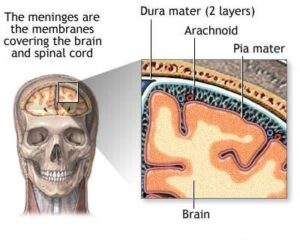
The meninges consist of three layers: dura mater, arachnoid mater, and pia mater. These layers protect the brain and spinal cord and contain blood vessels that can become inflamed during a migraine, increasing pain sensitivity.
Temporomandibular Disorders (TMDs) and Headaches
TMDs are closely associated with headaches, occurring in over two-thirds of TMD patients. The overlap in symptoms, such as joint pain, muscle tension, and neck pain, intensifies the severity and frequency of headaches. Early management of TMD can help reduce the chronic pain cycle that often exacerbates these headaches.
Role of Head and Neck Muscles
Tension in the head and neck muscles can trigger migraines by causing misalignments in the cervical spine, known as subluxations. This irritation of nearby nerves worsens headache symptoms by sending additional pain signals to the brain.
Conditions like occipital neuralgia, which involve inflammation or injury to the occipital nerves, can also contribute to severe headaches or migraine-like symptoms. These nerves, originating from the upper cervical spine, transmit pain signals from the neck to the scalp and can cause sharp, stabbing pain behind the eyes or at the base of the skull. Cervicogenic headaches, which mimic migraines, are often caused by issues in the neck, particularly the C2-3 joints.
Effective Home Remedies and Lifestyle Changes for Managing Migraines
To help manage migraines at home, consider trying these practices for immediate relief and long-term prevention:
- Rest in a quiet, dark room: Close your eyes and take a break or nap when symptoms begin.
- Apply a cool compress: Use a cool cloth or ice pack wrapped in a towel on your forehead.
- Stay hydrated: Drink plenty of water to help reduce symptoms and prevent dehydration.
- Relaxation techniques: Practices like biofeedback can teach you how to manage stress, which could help reduce the frequency of migraines.
- Set a routine: Try to keep a consistent sleep and eating schedule. Avoid sleeping too much or too little, and aim to eat meals at regular times every day.
- Stay hydrated: Drinking plenty of water can help prevent dehydration, which may trigger migraines.
- Keep a headache diary: Tracking your symptoms can help identify migraine triggers and effective treatments. This information will also help your healthcare provider monitor your progress.
- Exercise regularly: Aerobic activities like walking, swimming, or cycling can reduce tension and lower the risk of migraines. Be sure to warm up properly, as sudden, intense exercise can trigger headaches. Regular exercise also helps maintain a healthy weight, which may be beneficial since obesity is thought to contribute to migraines.
Headache Relief and Migraine Treatment in NYC
At Prestige Health and Wellness, the clinic takes a comprehensive, personalized approach to treating headaches and migraines. The goal is not just to alleviate immediate symptoms but to address the issue’s root causes and improve long-term health. Treatments are tailored to meet each patient’s unique needs using various therapeutic modalities.
Chiropractic Care for Headaches and Migraines
One of the cornerstones of treatment at Prestige Health and Wellness is chiropractic care. Chiropractors focus on spinal misalignments, or subluxations, that can contribute to headache and migraine development. Through precise spinal adjustments, chiropractors restore alignment and reduce strain on the nervous system, often resulting in fewer and less intense headaches. Particular emphasis is placed on the upper cervical spine due to its strong connection to migraine triggers.
Techniques like the Gonstead method target this region to improve function and potentially reduce migraines. Soft tissue therapies, such as massage and myofascial release, are also incorporated to relieve neck and shoulder tension, helping ease headache pain further.
Acupuncture for Pain Relief
Acupuncture is another integral part of the clinic’s holistic approach to migraine management. This technique stimulates specific points on the body, which can help address energy imbalances contributing to tension headaches or migraines. Acupuncture complements the other treatment methods by promoting pain relief and enhancing overall well-being.
Physical Therapy and Posture Correction
Physical therapists at Prestige Health and Wellness focus on strengthening the neck and upper back muscles, which can help reduce the muscle tension that often triggers headaches. They also work with patients to improve their posture, which plays a crucial role in preventing tension headaches. By combining physical therapy and ergonomic guidance, patients gain tools to improve mobility and reduce headaches.
Nutritional and Lifestyle Support
In addition to hands-on therapies, Prestige Health and Wellness offers nutritional counseling to help patients identify and avoid potential dietary triggers that could be contributing to their migraines. The clinic also provides lifestyle guidance, assisting patients in managing stress and modifying daily activities that may worsen headaches. This comprehensive approach ensures that all aspects of a patient’s health are considered when managing their condition.
Overall, Prestige Health and Wellness offers a multi-faceted, individualized treatment plan that addresses both the immediate symptoms and long-term health goals of those suffering from headaches and migraines. By combining chiropractic care, acupuncture, physical therapy, and lifestyle modifications, patients receive a balanced, holistic approach to wellness.
Contact Us
If you’re struggling with migraines or tension headaches, don’t wait—schedule an appointment today at Prestige Health & Wellness in Manhattan. Our expert team specializes in chiropractic treatments for migraines and headaches, physical therapy, occupational therapy, acupuncture, and massage therapy. We offer personalized care to alleviate symptoms and address the root causes of your pain.
Visit us at our convenient locations in Midtown, the Financial District, Hudson Yards, Chelsea, or Nomad to start your journey toward relief and improved well-being.
Sources
- Cleveland Clinic. Chronic Migraine. April 1. 2023. https://my.clevelandclinic.org/health/diseases/9638-chronic-migraine
- Di Paolo, C., D’Urso, A., Papi, P., Di Sabato, F., Rosella, D., Pompa, G., & Polimeni, A. (2017). Temporomandibular Disorders and Headache: A Retrospective Analysis of 1198 Patients. Pain research & management, 2017, 3203027. https://doi.org/10.1155/2017/3203027
- National Institute of Neurological Disorders and Stroke. Migraine. https://www.ninds.nih.gov/health-information/disorders/migraine
- Pescador Ruschel MA, De Jesus O. Migraine Headache. [Updated 2024 Jul 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560787/
- Pilitsis, Julie G. Occipital Neuralgia. American Association of Neurological Surgeons. April 30, 2024. https://www.aans.org/patients/conditions-treatments/occipital-neuralgia/



